Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms
re: Are Latent Viruses Causing Long Covid-19 Symptoms? Patient Groups Push for Testing
re: SARS-CoV-2 infection and persistence throughout the human body and brain
Real science is never settled, and anyone who has certainty on such things is not qualified to discuss it.
See my previous coverage of Long Haul COVID, from which I am still suffering, with my physical ability fluctuating between 10% and 20% in comparison to my typical fitness this time of year.
PASC = Posty-Acute Sequelae of COVID-19
ME/CFS = myalgic encephalomyelitis / chronic fatigue syndrome
Some PASC patients meet the diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) – a neuroinflammation-linked condition characterized by a range of debilitating chronic symptoms including severe fatigue, musculoskeletal pain, and post-exertional malaise.
Yep, all three for me, and more.
See also: Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation and SARS-CoV-2 infection and persistence throughout the human body and brain
Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms
23 June 2021. Emphasis added. See also the PDF version.
The novel virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a pandemic of coronavirus disease 2019 (COVID-19). Across the globe, a subset of patients who sustain an acute SARS-CoV-2 infection are developing a wide range of persistent symptoms that do not resolve over the course of many months.
These patients are being given the diagnosis Long COVID or Post-acute sequelae of COVID-19 (PASC). It is likely that individual patients with a PASC diagnosis have different underlying biological factors driving their symptoms, none of which are mutually exclusive. This paper details mechanisms by which RNA viruses beyond just SARS-CoV-2 have be connected to long-term health consequences. It also reviews literature on acute COVID-19 and other virus-initiated chronic syndromes such as post-Ebola syndrome or myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) to discuss different scenarios for PASC symptom development.
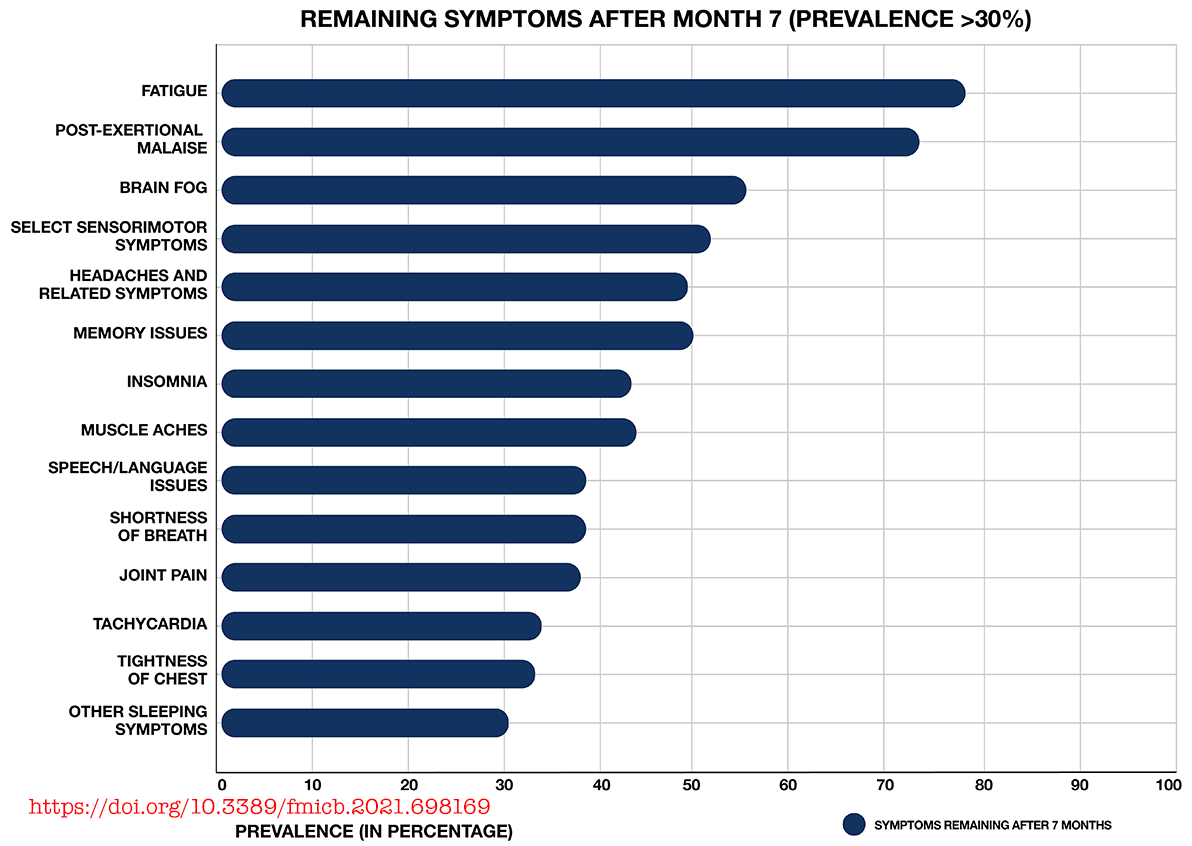 Most common symptoms remaining after 7 months in 966 respondents from a cohort of suspected and confirmed COVID-19 cases.
Most common symptoms remaining after 7 months in 966 respondents from a cohort of suspected and confirmed COVID-19 cases.
Results obtained via an international web-based survey. Image adapted with permission from Davis et al. (2020).Potential contributors to PASC symptoms include consequences from acute SARS-CoV-2 injury to one or multiple organs, persistent reservoirs of SARS-CoV-2 in certain tissues, re-activation of neurotrophic pathogens such as herpesviruses under conditions of COVID-19 immune dysregulation, SARS-CoV-2 interactions with host microbiome/virome communities, clotting/coagulation issues, dysfunctional brainstem/vagus nerve signaling, ongoing activity of primed immune cells, and autoimmunity due to molecular mimicry between pathogen and host proteins.
The individualized nature of PASC symptoms suggests that different therapeutic approaches may be required to best manage care for specific patients with the diagnosis.
...across the globe, a subset of patients who sustain an acute SARS CoV-2 infection are developing a wide range of persistent symptoms that do not resolve over the course of many months (Carfì et al., 2020; Davis et al., 2020; Huang C. et al., 2021) (Figure 1). One study of COVID-19 patients who were followed for up to 9 months after illness found that approximately 30% reported persistent symptoms (Logue et al., 2021). These patients are being given the diagnosis Long COVID, post-acute COVID-19 syndrome (PACS), or post-acute sequelae of COVID-19 (PASC).
Post-acute sequelae of COVID-19 is being diagnosed in patients who developed severe acute COVID-19, but also in patients who experienced only mild or asymptomatic cases...
... While the development of long-term symptoms following SARS-CoV-2 infection is sometimes framed as novel or mysterious, it is actually an expected phenomenon. Most well-studied viral or bacterial pathogens have been connected to the development of chronic symptoms in a subset of infected patients...
Some PASC patients meet the diagnostic criteria for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) – a neuroinflammation-linked condition characterized by a range of debilitating chronic symptoms including severe fatigue, musculoskeletal pain, and post-exertional malaise (worsening of symptoms following exertion) ...
[WIND: precisely, all of those things persist for me]...Pathogens most commonly implicated in ME/CFS development include neurotrophic herpesviruses and enteroviruses...
It is likely that the different pathogens implicated in ME/CFS development are capable of dysregulating host gene expression, immunity, and metabolism via similar mechanisms, leading to similar sets of chronic symptoms in ME/CFS-diagnosed patients...
[WIND: yes: I gained 25 pounds in 25 weeks!]...
It is also possible that, at least in some PASC patients, SARS-CoV-2 may drive chronic symptoms by persisting in certain body sites or tissue reservoirs after acute infection. A growing number of studies show that some patients infected with SARS-CoV-2 do not successfully clear the virus over long periods of time...
Another possible scenario for persistent symptom development in some PASC patients is that SARS-CoV-2 may fully clear from patient blood, tissue and nerves after acute infection. However, the virus may dysregulate the host immune response during acute COVID-19 in a manner that allows previously harbored pathogens to reactivate, infect new body sites, and drive new chronic symptoms.
It is well understood that humans accumulate persistent viruses over the course of a lifetime. These viruses generally persist in dormant, latent, or non-cytolytic forms, but may reactivate under conditions of stress or immunosuppression. Indeed, people regarded as healthy have been shown to harbor a wide range of persistent viruses in blood, saliva, or tissue that are capable of activation under such conditions...
Like viruses, many bacterial, fungal, and parasitic pathogens also change their activity and/or infect new tissue and the CNS under conditions of immune dysregulation or stress. These include tick-borne bacterial pathogens such as Borrelia burgdorferi, Rickettsia, and Bartonella henselae...Approximately one third of the world’s population harbors Toxoplasma gondii (T. gondii), a parasite that can differentiate into a latent form that establishes persistent infection in muscle and brain tissue...
...Thus, any PASC patient with multiple ongoing inflammatory issues would be expected to suffer from increased mast cell and glia-related immunopathology. This “primed” state may also be an important part of symptoms like sensory sensitivity in some individuals who have survived an acute neuroinflammatory event such as encephalitis or concussion, or who may have low levels of persisting or latent neurotropic pathogens.
...Another mechanism by which SARS-CoV-2 may promote PASC symptoms is by activating the host immune response in a manner that leads to long-term autoantibody production. Several research teams have isolated a range of autoantibodies in acute COVID-19 patients... SARS-CoV-2 itself has been shown to drive cross-reactive antibody responses. For example, Kreye et al. (2020) identified high-affinity SARS-CoV-2-neutralizing antibodies that cross-reacted with gut, kidney, lung, heart, and brain mammalian self-antigens. Antibody binding in the brain occurred in the basal ganglia, hippocampal formation, olfactory bulb, and cerebral cortex...
...Many patients given a PASC diagnosis report a spectrum of symptoms that either meet the diagnostic criteria for ME/CFS, or are very similar in nature to those suffered by ME/CFS patients. These symptoms include dysautonomia, diffuse pain, sleep problems, flu-like symptoms, trouble concentrating, and nausea. The central role of the brainstem in the sickness behavior response, autonomic control, and arousal suggests that dysfunctional brainstem signaling may be an important driver of PASC symptoms that overlap with those of ME/CFS... including one study demonstrating brainstem glial activation positively correlated with cognitive impairment.
...
WIND: scary as shit. It all dovetails with my personal observations. I don’t want to live out my days with the way things stand, so I will continue to focus on nutrition and hope for some medical salvation.
A year ago I was already speculating on brainstem/vagus nerve disfunction (particularly lung function) as well as auto-immune issues (Hashimoto’s Thyroiditis and rheumatic symptoms), brain fog and headaches, 4 months of gastrointestinal problems (“interactions with host microbiome/virome communities”), weight gain of 25 pounds in 25 weeks, and Epstein Barr virus.
The “persistent reservoirs of SARS-CoV-2 in certain tissues” is an interesting one. If it can be shown that the virus can be harbored longer-term, then I would be much more open to the idea that the vaccine could help, in the hope of killing it off.
The autoantibody effects are most concerning:
Under such conditions, “autoantibody” production would vary widely between different COVID-19 patients. That is because the composition and virulence of patient microbiome/virome communities capable of contributing to cross-reactive “autoantibody” production differs greatly among individuals. The same is true of persistent pathogens capable of reactivation in COVID-19 tissue. Moreover, SARS-CoV-2 infects different body sites and cell types in different patients.
This model fits with the Wang et al. (2021) COVID-19 “autoantibody” findings. The team was unable to identify COVID-19 “autoantibody” responses that could extensively partition patients into specific phenotypes or outcomes. Instead, they observed an extensive constellation of rare and uncommon “autoantibody” reactivities with large apparent effect sizes. This led to the conclusion that “relatively private reactivities are common in COVID-19, and the aggregate sum of these multifarious responses may explain a significant portion of the clinical variation in patients.” In some patients, this varied “autoantibody” production might continue after resolution of acute COVID-19 disease, leading to PASC symptoms.
But effects on the brain... I had that in spades for 7 months, and I still get mild headaches.
Many patients given a PASC diagnosis report a spectrum of symptoms that either meet the diagnostic criteria for ME/CFS, or are very similar in nature to those suffered by patients. These symptoms include dysautonomia, diffuse pain, sleep problems, flu-like symptoms, trouble concentrating, and nausea. The central role of the brainstem in the sickness behavior response, autonomic control, and arousal suggests that dysfunctional brainstem signaling may be an important driver of PASC symptoms....