Can an Extreme Endurance Athlete Have an Early Heart Attack? CT Coronary Calcium Scan, HDL Cholesterol, LDL Cholesterol, Statins, Atherosclerosis, etc (UPDATE with a cardiologist viewpoint)
Legal disclaimer: since we are not doctors, do NOT follow anything based on health-related topics on this or related sites without first consulting with your doctor or other trusted health professional.This is NOT medical advice and we are not qualified in any way to offer medical advice.
Update: coronary artery calcification might well be the result of magnesium deficiency and/or Vitamin K2 deficiency in many cases, those deficiencies preventing excess calcium from going into bones and allows it to build up within the body, including arteries.
UPDATE 2021-01-02: Cardiac Stress Test Echocardiogram up to Max Heart Rate, with a Surgical Mask
....
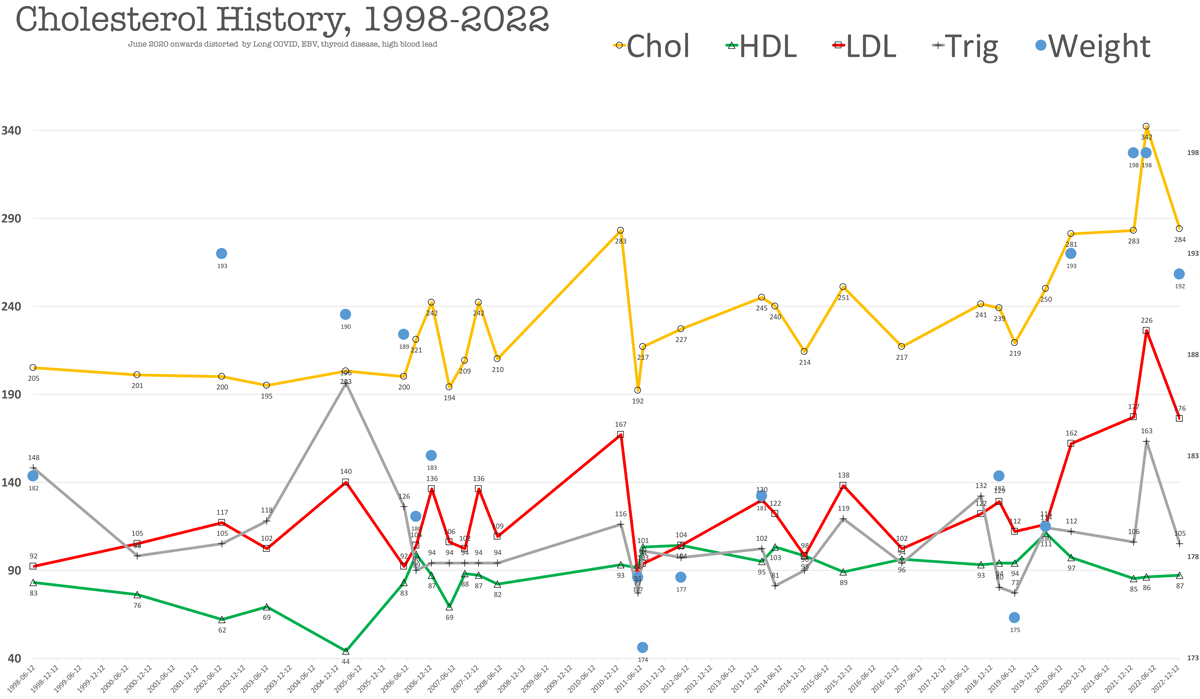
A new challenge: reversing early arteriosclerosis. I think I may have to get down to 5% body fat to see if it can be done. There is no consensus on whether getting body fat that low can reverse arterial plaque. My working theory is that the body will scavenge soft plaque), but I do know that when I was at 8% body fat with only 1 pound of visceral fat (!), my cholesterol was the lowest it had ever been over a period of 22 years—see the graph.
The core problem I face in researching this issue is that as a layman, sorting through conflicting expert opinions is difficult. What is clear is that the evidence for heart disease root causes is exceedingly weak, and based on epidemiological studies of large numbers of mostly obese people who never exercised and ate garbage all their lives (e.g. Americans—just go visit Walmart one day!).
Worse, the link to diet is weak to say the least, let alone the role of the microbiome, exercise, genetics, epigenetics, etc. Given the fiascoes in nutrition revealed in recent years by new research, it is very hard to accept any recommendations as having merit. Heck, medical science can’t even figure out trivially simple (by comparison) glycemic index, which varies hugely for the same food for different people.
Note: numbers from 2020 onwards were in the throes of extreme Long-Haul COVID symptoms, later years screwed up from EBV and thyroid issues and high blood lead, and carrying an excess 20 pounds of body fat and not being able to exercise normally
Background
Just under two years ago in late March of 2018 I had a CT Coronary Calcium Scan which showed arteriosclerosis placing me in the 81st percentile for my age (mid 50's), the 99th percentile being the worst, 0th the best. Meaning that out of 100 men, 88 or so would have less arterial plaque for my age.
LAD = left anterior descending artery
March 2019
Visual assessment of the coronary arteries shows moderate coronary artery calcification centered within the LAD. Quantitative calcium score provided by the 3D Lab is 91.2, which places the patient in the 81st percentile for age and gender.
Heart: normal in size, no significant valvular calcification.
Pericardium: no pericardial effusion.
Pulmonary arteries: not enlarged.
Thoracic aorta: no significant abnormality
Less than a year later, there appears to be a huge increase in calcifiation from 91.2 to 159—I’m not sure of the scale, but it sure sounds bad (a 74% increase).
February 2020
Visual assessment of the coronary arteries shows calcification of the LAD, circumflex, RCA, and diagonals. Quantitative calcium score provided by the 3D Lab is 159. Moderate plaque burden with a calcium score of 159, which places the patient in the 84th percentile for age and gender.
Specific artery assessments are as follows:
Left Main (LM): 0
Left Anterior Descending (LAD): 132
Left Circumflex (LCX): 5.58
Right Coronary Artery (RCA): 21.4Heart: Normal in size. No significant valvular calcification.
Pericardium: no pericardial effusion.
Pulmonary arteries: not enlarged.
Thoracic aorta: no significant abnormality.
All this is a shocker, given my exercise and diet, but I seem to have inherited a genotype or have had epigenetic triggers or a gut microbiome that is unfavorable for cholesterol (update: magnesium deficiency?). See my 22 year cholesterol chart further below, which suggests that it’s pretty much the way my body works.
The CT calcium scan is not very helpful, so I am looking into a heartflow scan. Do I have 10% blockage, 30%, what? No meaningful risk assessment can be made with such vague information IMO, particularly in weighing against all the potential downsides of statins, which appear to be much higher than the medical industry wants to acknowledge, and such risks are always framed in epidemiological terms which means mainly high risk people who never exercised much or at all, and ate badly as a life habit. And... maybe it is all about inflammation and sugar and has nothing to do with dietary cholesterol.
I’m willing to do what it takes to halt and hopefully reverse arteriosclerosis, but the more questions I ask, the more I find that doctors have no idea how to do that! Meaning it’s all vague recommendations that on average might help. But the more I learn about the gut microbiome, the more I think that much of that is averaged-out epidemiological bullshit for any particular individual. Basically, the science is crap when it comes to an individual cases and there isn’t even agreement on the side effect profile. So how do I assess if I’m going to collapse and die of a heart attack in five or ten years and weigh that against the risks that no one can properly assess?
Seems like one huge guinea pig experiment: New Study Adds to Debate Over Statin Use to Prevent CVD
The authors consistently found that the harms outweighed the benefits until 10-year CVD risk thresholds substantially exceeded those recommended in current guidelines... anywhere from 50 to 200 people who don’t have CVD must take a statin to prevent just 1 heart attack over 5 years. Meanwhile, many of these patients will develop muscle pains and they are also at higher risk of developing type 2 diabetes.
Moreover, studies I’ve found suggest that the majority of pro athletes cannot tolerate statins. What does that say for me, doing double centuries and the training for it? Moreover, statins can attenuate fitness gains and fitness gains can offset the risks from high LDL.
Worse, how does one make intelligent choices without monthly lipid profiles to see what works and what doesn’t? Good science means changing one variable and seeing if it helps (e.g., using psyllium husk @AMAZON or oatmeal or whatever for a month, or dropping 10 pounds of body fat, etc). I have had exceptional dietary discipline before (recording food to the gram, etc), but more than a month is discouraging without feedback.... are the changes working for me or not? That is the massive flaw in the whole system.
Data for 2020-02-14 shows HDL (good) cholesterol level of 111 mg/dL, which is sort of off the charts. While HDL is called “good cholesterol” for its scrubbing of LDL cholesterol, the latest science now ponders if too much HDL may be associated with increased risk of heart attack and death:
...more research is needed to elucidate the mechanisms of this paradoxical association. "While the answer remains unknown, one possible explanation is that extremely elevated HDL cholesterol may represent 'dysfunctional HDL' which may promote rather than protect against cardiovascular disease," he said.
I know that my HDL rises the more I lose body fat, while LDL decreases. This seems paradoxical, just as the above states. But could my latest HDL of 111 (extremely high) be associated with LDL, sort of rising in tandem? That would violate past patterns in which HDL rise is associated with LDL decrease. Go figure.
Statin?
Last week my internist said I would likely have a heart attack within 7 years if I did not get my LDL cholesterol down (further buildup). ALL other tests are poster-perfect including blood pressure of 116/68.
All of my doctors say I should be on a statin. A statin is a medication that reduces cholesterol with alleged reductions of 24% to 36% reduced risk of heart attack, which is not much IMO and why the hell the wide range? Seems sketchy at best.
I am loathe to take a statin because the “rare” side effects are likely not so. I know from personal experience with Metronidazole that doctors DO NOT report adverse effects properly, or at all. So statistics on side effects are almost certainly total bullshit. And for those in poor health (most), side effects are both less important and less noticed and maybe a reasonable tradeoff.
My specific concerns with taking a statin are :
- Risk of nerve inflammation. After severe nerve damage from Metronidazole that took two years to recover from, the least thing I want in my body is anything that carries any risk of nerve damage.
- Cognitive impairment—years from now maybe we’ll find that dementia and similar are made worse by statins. Statins can affect cognitive function (“reversible cognitive impairing effect in some patients”, “clinical trials were not originally designed to detect cognitive impairment”) but science is in doubt as to benefit or impairment. And with my brain finally mostly back in order after a concussion, the last thing I want is to fuck it up with a statin or find out that “reversible” is really a lie from big pharma—big money means bigger lies.
A double blind placebo-controlled trial of lovastatin’s effect on cognitive functioning and mood showed detrimental effects on cognitive performance on four neuropsychological tests assessing attention, working memory, and overall mental efficiency... Post-marketing surveillance has continued to uncover case reports of cognitive effects associated with statin use since the FDA report
- 100% to 200% increased risk of diabetes with some statins.
- Risk of life threatening muscle damage with some statins; rare but one drug was withdrawn from the market for that reason. Or just muscle aches and pains, a total non-starter for me as an athlete.
- Liver inflammation—what does a statin do to the liver during extreme stress such as in a double century? I doubt there is any science at all on such things.
Scientific studies
Scientific studies are so dubious these days: there is disconcerting evidence of sloppy work or money involved 75% of the time. So call me a skeptic on statins and the $billions involved in selling statins to millions of obese sedentary people, versus someone like myself doing double centuries and exercising 10 times as much every day as most of those statistical people do in a week.
While every doctor I’ve seen (two internists and a cardiologist) have recommended a statin to me, no doctor has ever offered a credible risk assessment of the side effects of statins, or even brought the issue up. That’s a huge red flag, a “halfpinion”—it’s bad science, bad medicine, bad risk management to offer a “solution” without also considering the negatives.
No one is an epidemiological statistic. A recommendation that works on average—that’s like saying every woman is 13.7% pregnant, which is obviously idiotic. Some people are damaged by some medications, sometimes fatally. What I want is a tailored personal recommendation based on my lifestyle, my genetics along with my current gut microbiome, my diet. But that doesn’t exist AFAIK with regards to arteriosclerosis.
Every person responds differently to medications, as I learned the hard way. PLUS, I am an extreme outlier with respect to epidemiological statistics for arteriosclerosis, as follows:
- I am an ultra endurance athlete.
- I have been active nearly all my life.
- I regularly take my body fat to 10% or so, sometimes lower.
- I have an off-the-chart HDL cholesterol of 111 out of a 250 total cholesterol. Medical science cannot agree on how protective this “good” HDL cholesterol is, but I am certainly several standard deviations away from any normal.
- Both my parents are at or near 80, and have never had a heart attack or stroke. My mother has high cholesterol, my father’s is very good.
- I eat a far healthier diet than most Americans. my diet being 100% free of cheeseburgers and sodas and processed foods and the garbage that most people eat. I eat the good stuff. My main dietary failing is having eaten 2-3 quarts of full-fat Greek yogurt the past 5 months, a great travel food when burning an extra 2000 calories a day in the cold.
How I plan to handle it
Update June 2020: magnesium supplementation with a highly bioavailable form.
I am strongly averse to a statin, which aside from the risk discussed above, seems like a bad idea without first making all reasonable efforts on diet and body fat, which do not carry risks.
- Reduce body fat by 10 pounds to get to 8% body fat. I have done this before, so it can be done.
- (stretch goal) Get to 5% body fat in hopes that this will REVERSE arteriosclerosis.
- Increase consumption of psyllium husk, oatmeal. Add 4000 mg omega 3. Continue olive oil and similar friendly oils, avocado, etc. These items together in theory could cut blood cholesterol by 20% or more.
- Reduce consumption of whole fat yogurt to no more than one quart per week.
- Continue with favorable diet for gut microbiome including
Based on past assessments, achieving 8% body fat should drop total cholesterol to 190 or so (2011-05-20 in graph). Since I cannot maintain that low level of body fat, I will have to rely on diet for most of the year.
See also
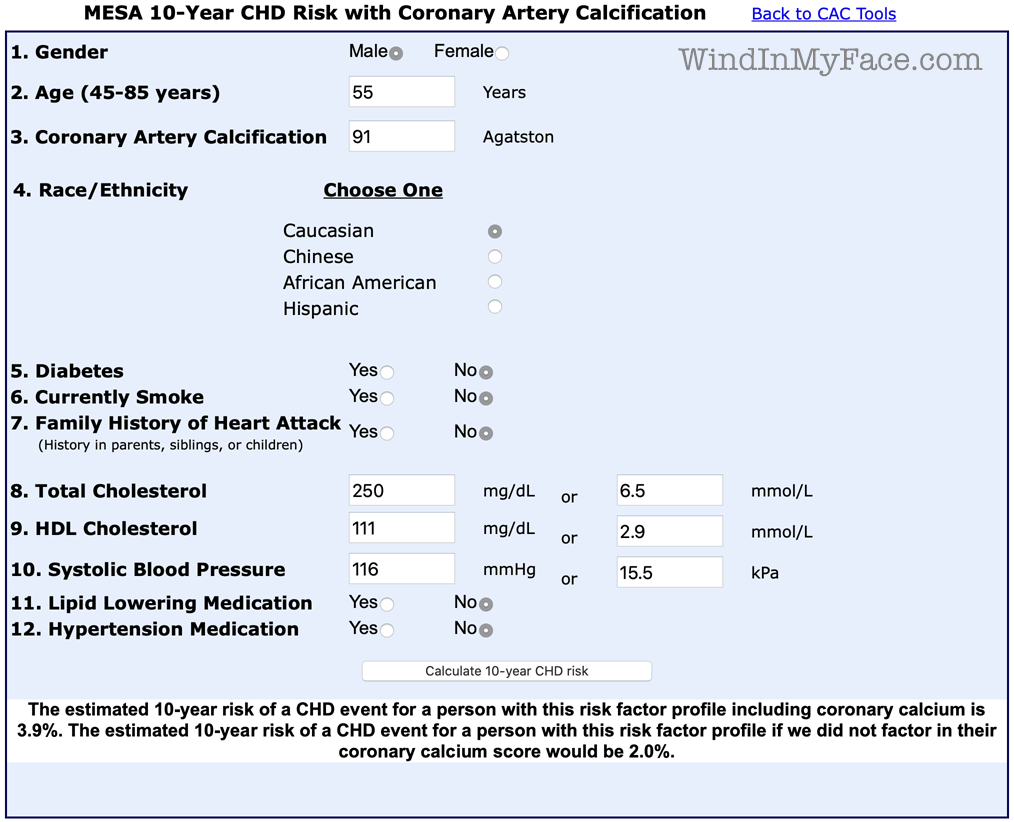
MESA 10-Year CHD Risk With Coronary Artery Calcification
ACCEL: Detecting CAD in Older Athletes and What to Recommend When You Find
Expert Opinion: Fat for Thought – Any Role for the Ketogenic Diet in Athletic Training?
Cardiologist viewpoint
Emphasis added.
From Jon L (a recently retired academic cardiologist).
“Can endurance athletes die of premature heart attack?”
The answer is yes. Perhaps the most notable case is that of the runner Jim Fixx. From Wikipedia:
“Fixx died on July 20, 1984 at age 52 of a fulminant heart attack, during his daily run on Vermont Route 15 in Hardwick.[1] The autopsy, conducted by Vermont's chief medical examiner, Dr. Eleanor McQuillen, revealed that atherosclerosis had blocked one coronary artery 95%, a second 85%, and a third 70%.[4] (His father Calvin Fixx had died of a second heart attack at age 43.[5])
“In 1986 exercise physiologist Kenneth Cooper published an inventory of the risk factors that might have contributed to Fixx's death.[6] Granted access to his medical records and autopsy, and after interviewing his friends and family, Cooper concluded that Fixx was genetically predisposed - his father died of a heart attack at 43 after a previous one at 35, and Fixx himself had a congenitally enlarged heart - and had an unhealthy life: Fixx was a heavy smoker before beginning running at age 36, had a stressful occupation, had undergone a second divorce, and his weight before he took up running had ballooned to 214 pounds (97 kg).[7] Medical opinion continues to uphold the link between moderate exercise and longevity.[8]”At issue is what risk any individual has for developing atherosclerotic vascular disease (ASVD). Risk is assessed using data from population studies (“derived from pooled cohort estimates”). As you suggest, endurance athletes are poorly represented in these pooled cohorts. Given the fact that exercise is generally accepted as reducing risk of ASVD, risk assessed using these tools may overestimate risk for endurance athletes. Although it is generally accepted that moderate exercises reduces cardiovascular risk, there is evidence that this benefit diminished with the highest levels of exercise (most notably in marathon runners).
In contrast to Fixx, the estimate of your risk, based on the data you have provided (age, gender, cholesterol levels, negative family history of premature disease, etc,) would be on the order of 2% which is considered low. Even adding your coronary calcium score, (which would not be recommended in your case given the low basal risk), your risk would still be considered low (3.8% with ≤ 5% considered low risk).
The presence of coronary calcification indicates the presence of atherosclerosis. Recent studies suggest that the prevalence of coronary calcification is higher in endurance athletes, and that coronary calcification scores may be elevated in response to vigorous exercise. These studies are not large enough to clearly establish whether the increased coronary calcium was associated with an increase in ASVD events. See DeFina et al, JAMA Cardiol, 2019;4(2):174-181. Association of All-Cause and Cardiovascular Mortality With High Levels of Physical Activity and Concurrent Coronary Artery Calcification. Additional studies with CT angiography suggest that these lesions are more densely calcified, thought to be more stable, and less likely to rupture and cause an event.
You correctly point out that our understanding of the pathogenesis of ASVD remains incomplete. There is good evidence to support the presence of diabetes, hypertension, chronic kidney disease, unfavorable cholesterol levels, smoking and family history as major risk factors for premature ASVD. Current research is focused on the role of the gut microbiome, inflammation and other factors. The role of gut microbiome is being addressed by informatics and analysis of large datasets (stool DNA analysis) where the role of artificial intelligence may come to into play.
As regards your high levels of total cholesterol, the significance is offset by the high HDL cholesterol, normal LDL cholesterol and triglycerides.
You raise the question of what further tests might be considered to refine further your individual risk of premature ASVD. Assessment of coronary blood flow by myocardial perfusion imaging would be of limited value given your low pre-test likelihood and excellent exercise tolerance. Elevation of high-sensitivity C-reactive protein (hs-CRP) has been used as a marker of subclinical inflammation and has been considered to provide additional information as to risk. Asymptomatic individuals with elevated hs-CRP have been shown to benefit from statin therapy with a reduction in ASVD events (Jupiter trials). This finding has not been assessed in endurance athletes.
The next question is how would the results of additional testing change the approach to further risk reduction. Some authorities would recommend statins. However, given your overall low risk, the benefit of statins might be expected to be low. Moreover, as you correctly point out, statins are not well tolerated in athletes. Similarly, aspirin which has proven benefit in patients with manifest ASVD events, would not be indicated for you given that the risk of increased bleeding would outweigh any potential benefit (particularly if you had another bike crash while cycling!).
All of the aforementioned discussions are predicated on the information you have provided. As indicated in the 2019 AHA/ACC Guidelines for Primary Prevention of ASVD, shared decision making between you and your doctors should determine the best strategies top reduce your risk. Your case is further complicated by the lack of clear data for high endurance athletes. Moreover, our current health care systems do not provide physicians the time to have detailed discussion of the relative risks and benefits of interventions with their patients (and may in fact penalize the physician if they “…spend too much time…” with a patient. Many patients are looking for a pill to fix their problem and they are rewarded with a statin. The patient is happy because he got a pill and the physician is happy because he has done something to meet the patient’s expectations. Additionally, should the patient have an atherosclerotic event, the physician would not be faced with the question “Why didn’t you start the patient on a statin?”.
For now, the most important thing would be to watch for unexplained changes in your exercise tolerance, shortness of breath or the development of new chest tightness. The onset of new symptoms or decrease in exercise tolerance should prompt further cardiac evaluation. Continued extreme exercise does carry some risk of a cardiac event, but there is little compelling evidence to suggest how that risk might be reduced further. Again, these recommendations should be considered relatively unique to your situation and not necessarily appropriate for other endurance athletes.
WIND: I felt vigorous at 14252' elevation (4344m) just last August, along with weeks spent at 10K to 12K feet last fall and hiking faster with a load than most people half my age... that the low partial pressure of oxygen would have a high likelihood of flushing out a heart blockage issue, particularly at max heart rate at 14K feet while sprinting to the summit. No issues whatsoever.
Making the available data even more tenuous, I am a cyclist and I wonder if runners could have different risks due to much higher impact and stress versus cycling. In cycling, the body when properly fitted and positioned acts as a shock absorbing spring, sparing the chest from stress. In a runner the stresses may be quite high if descending, but even on flat ground there is joint-killing pounding going on continually.
Another cardiologist weighs in:
Based on your numbers, I wouldn't put you on a statin. You're healthy, your HDL is excellent, and you have no family history of CAD. Trust me, I've saved way more lives putting people on statins than putting in stents. They are good and safe drugs. That being said, I wouldn't put on a statin. Sure, you've got some coronary calcium - it's not too uncommon - but I'd probably hold off for now. If you wanted the lowest cardiovascular risk, then you could take a statin, but with your family history and high HDL, I don't think you're entirely likely to benefit from it.
As an aside, getting down to that low of a body fat percentage is sketchy. the TdF riders that can do that only get that low briefly. The risk for illness and increased inflammation may be higher. I don't know, but be careful.
WIND: I have felt very healthy at 8% body fat, but I looked like a skinny teenager, and lower than that is probably risky.