Prelude
I’m on my 4th post-COVID year, prior to which I had done 55 double century rides, and competitively too, winning a smaller event here and there, and by soloing (no drafting). I state that to illuminate the extreme contrast between March 2020 and April 2024. I still don’t know if I’ll ever again be able to ride a century, let alone a double century.
Three “lost”years of my life*, and it still a struggle to get back some degree of fitness. At first it was a massive Epstein Barr onslaught (antibody tests escalating over 12 months) plus who knows what, then Hashimoto’s Thyroiditis (miraculously subsided). Things seem to be settling down, but I am 30 pounds over my spring training weight and that isn’t helping.
Here 4 years later I have greatly improved, but am a fractional self of pre-COVID. But in the first major positive sign, last autumn I was able to climb Mt Conness. A short and relatively easy climb (10 miles round trip, 2500 vertical), for ~3 years I could not have contemplated even the first mile of the flat approach, let alone the steep stuff. A huge win after years. That’s not saying I could do it at will; it was the culmination of weeks of things going well.
Positive vs Negative Energy Balance from Exercise
My challenge here in April 2024 is to get back into positive energy balance from exercise.
Positive Energy Balance — a virtuous cycle
For most of my life, exercise tired me while doing it (eventually), but the feel-good aspects both during and after exercise feeling and the resulting boost in overall energy and feelings of well being made it a positive energy balance. More please!
With healthy physiology, exercise is a virtuous loop whereby more exercise (in proper measure) means even more energy, up to and including double century rides for me (loved 'em!). I was a powerhouse for much of my life. I did not tire easily or until after a very very long time. If you’ve ever felt that, then you’ll know just how awesome that feels.
Then events take that away.
Negative Energy Balance —exercise consistently nets-out at less
What if the 'reward' for exercise is punishment by days or even weeks of low energy malaise? No matter what you do, exercise means a net drain of physical and mental energy.
And what if you can no longer gauge how much is enough or too much? What if feeling really good on that rare day is a good sign but also blindness to what’s coming? A feedback loop that doesn’t work, misleads, betrays? That’s where it still sits for me. It is the opposite of my carefully honed sense of self for the rest of my life—and very hard to adapt to.
For most of the past 3 years most of the time, exercise took sheer force of will, like using The Force to make the body go. It felt as if my brain were under extreme duress, a draining almost painful concentration. And lacking any endorphin reward as with normal physiology, more like anti-endorphin. The most unpleasant anything I’ve ever done including the most strenuous double century in its last miles in extreme heat. Like pain but much worse. Makes you never want to try again. Having done 55 double centuries in all manner of conditions, I am not exactly afraid of fatigue or discomfort. But this process was godawful.
Rewards slow to come and reversals frequent. Negative energy balance with negative feedback is a very deep hole to climb out of.
Oscillating about the zero point
With 3+ years of net drain energy from exercise, I now feel that I’m oscillating about the zero point—approaching a neutral status where I am at least not losing net energy. But it’s also not yet a gain, not a positive energy balance.
A 45 minute easy ride (nothing approaching a hard effort!) might cost me 4 hours of my day from energy drain. Or another day, a 90 minute ride (again, easy) might be fine until an hour after then... wham. Or it might be fine. The feedback loop is unpredictable.
Or that infrequent and wondrous joyful day: a really good ride “like the old days” ride in which I feel stronger and stronger to the end. Not at full fitness, but at full operational status, the lungs and legs and heart all working beautifully like they ought. And yet within an hour the body collapses and an hourlong nap is needed just to feel functional. Then 10-12 hours of sleep. Maybe good sleep and maybe disrupted (another violation of the normal physiology of exercise supposedly helping sleep, more like requiring but not necessarily helping). And maybe the body physiology won’t work that well again for a month or three.
Pyschologists say that the unpredictablity of rewards is more reinforcing than predictable rewards, but I say that’s bullshit in this case.
What’s the alternative, giving up? Can’t do; the quality and duration of my life depends on it.
Exit the Sedentary?
I wonder if it feels this way for someone who has been sedentary for life? I’d guess that it might be like that for a month or so, then the reward system kicks in? No idea.
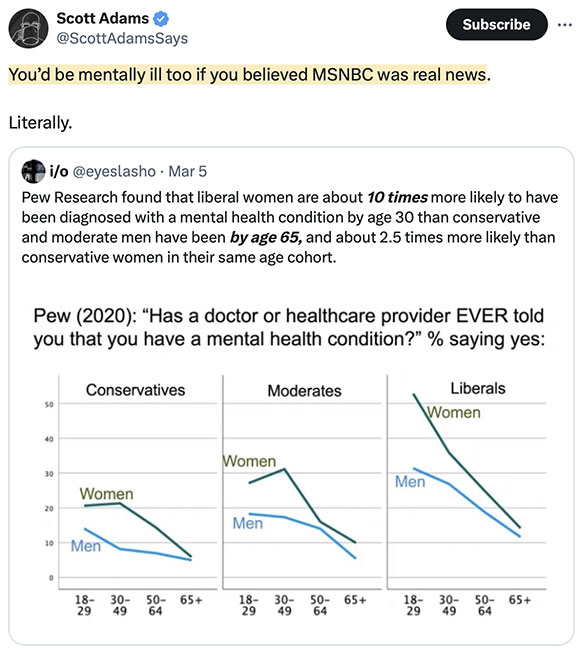
It’s bad enough that temperature stations are the very embodiment of anti-science.
If all else fails, just make shit up.
The real number is almost certainly closer to 50%, but whatever...
Hundreds of ‘ghost’ climate stations are no longer operational; instead they are assigned temperatures from surrounding stations.
...rely in part on temperature readings from the United States Historical Climatology Network (USHCN). The network was established to provide an “accurate, unbiased, up-to-date historical climate record for the United States,” NOAA states, and it has recorded more than 100 years of daily maximum and minimum temperatures from stations across the United States.
The problem, say experts, is that an increasing number of USHCN’s stations don’t exist anymore.
“They are physically gone—but still report data—like magic,” said Lt. Col. John Shewchuk, a certified consulting meteorologist.
“NOAA fabricates temperature data for more than 30 percent of the 1,218 USHCN reporting stations that no longer exist.”
He calls them “ghost” stations.
Mr. Shewchuck said USHCN stations reached a maximum of 1,218 stations in 1957, but after 1990 the number of active stations began declining due to aging equipment and personnel retirements.
NOAA still records data from these ghost stations by taking the temperature readings from surrounding stations, and recording their average for the ghost station, followed by an “E,” for estimate.
...
WIND: there is no climate crisis. It’s a psyop that fools believe in, funneling trillions of dollars to the well-connected grifters, and increasing pain and suffering on the masses.
How to measure the temperature of the earth:
- First, go batshit crazy and pretend this is even possible, or ever will be.
- Take only the high temperature as somehow representative of what’s happening. Ignore daily variations; in other words don’t track anything meaningful eg an ambient energy methodology.
- Locate thermometers near concrete and jet exhaust eg airports.
- Have “experts” pound relentlessly on the burning planet.
If all else fails, just make shit up, “adjust” data, etc.
And they’re doing this right in front of you.
Got your science fair vehicle yet?